- 0044 (0) 207 351 8754
- [email protected]
- Royal Brompton Hospital - London
All young children cough and many wheeze. This inevitably leads to a visit to the GP and it is not uncommon for these children to receive multiple courses of antibiotics, which enhances the parents’ belief that there is something wrong with their child. Children are often said to have recurrent chest infections, when in reality they are having the usual number of upper respiratory tract infections (viral colds), but with accompanying lower airway symptoms. However with current diagnostic trends, many of these pre-school children are given the label of asthma, which can cause considerable parental anxiety and in a few cases even social stigmatisation. A proportion will also be prescribed inhaled steroids, following the message that inhaled steroids rather than antibiotics are the treatment of choice for these recurrent symptoms.
It is difficult to diagnose asthma in this age group. In the past, these children were diagnosed as having wheezy bronchitis, however use of the term bronchitis led to widespread use of antibiotics, despite the fact that almost all these episodes are caused by viral and not bacterial infections. In an attempt to encourage use of bronchodilators, it was then emphasised that wheezing equals asthma. This inevitably led to over-diagnosis, and with the British Thoracic Society guidelines emphasising the use of inhaled steroids for asthma prevention, many children have been put on steroids unnecessarily. Clearly the pendulum needs to swing back as the truth lies somewhere in the middle. Whilst most asthmatic children cough (and some do so without obvious wheeze), most children who cough do not have asthma. Furthermore, many parents report that their child wheezes, when what they are really describing are the harsh sounds of upper airway secretions in the back of the throat.
So how is asthma diagnosed in this age group? The history is usually the key and there are certain pointers –
• Family history of atopy – asthma, hay fever or eczema in a parent or sibling (ignore the elderly grandparent who has bronchitis).
• Personal history of atopy – genuine atopic eczema rather than the occasional patch of dry skin.
Pattern of wheeze – background daily or night-time symptoms, or exercise-induced symptoms, rather than the commoner pattern of symptoms only when the child has a viral cold.
Examination is usually normal and unhelpful. However the presence of Harrison sulci (indentation or concave shape of the lower ribs) indicates chronic respiratory difficulties and is significant. Plotting height and weight may be useful, as poor growth may indicate a more significant underlying condition such as cystic fibrosis.
Investigations are usually unhelpful. Children under 6 years of age are unable to perform lung function testing, which is unfortunate as spirometry is the best way of confirming the presence of airways obstruction. Although the committed allergist may disagree, skin prick testing in this age group is rarely helpful.
If symptoms are marked or atypical, referral to a paediatrician is warranted, particularly one with a respiratory interest. In some cases, further investigations may be performed to exclude less common diagnoses. Gastro-oesophageal reflux, a condition where stomach acid regurgitates back up the oesophagus (food-pipe) must always be borne in mind, as not uncommonly it manifests as recurrent cough and wheeze that has not responded to standard therapy.
The single best thing most parents could do to help their symptomatic child is to stop smoking. It is our duty to inform the parents of the harm they are inflicting on their children (and themselves). In addition, constructive advice should be given to try and help those who wish to give up the habit.
Bronchoconstricted (narrowed) airways need bronchodilators – but these should only be used on an ‘as required’ basis rather than automatically taken 3-4 times a day. Nowadays they should be administered through a spacer device with a mask. There are several of these available on prescription, smaller volume ones include the AeroChamber and Able Spacer, larger volume ones include the Volumatic and Nebuhaler.
There is no point using this method if a child is distressed and screams every time the mask is put on their face, as drug deposition becomes minimal. In those circumstances, a, nebuliser remains the only option, but fortunately this is not too common an occurrence. By 3 years of age, most children can use the spacer without the attached mask, which increases the efficiency of lung deposition. Bronchodilators given in syrup form are far less effective and probably not worth using, as the dose required orally, in order to have an impact inevitably leads to side effects.
A small minority of pre-school children will require regular prophylaxis. Inhaled steroids are not too effective for those children who have episodic viral wheeze. However in those with background troublesome symptoms who are using a bronchodilator several times a week, a trial of inhaled steroids is warranted. Again, these should be administered through a spacer device, with or without a mask depending on age.
Fortunately the prognosis is generally very good and most will outgrow their symptoms. However, although most wheezy infants do not turn out to have persistent childhood asthma, most asthmatics do start wheezing when young. If we had a reliable predictor of those who will develop asthma with eventual structural changes in the airways, we could then target aggressive early anti-inflammatory therapy. Since currently no such predictor exists, this form of preventive management will have to wait.
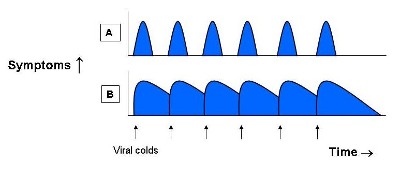
The shaded area represents times when a child is having symptoms, while the arrows represent each viral cold they catch. On average, the pre-school child gets 8-12 colds per year, mostly between September and March. In the top figure [A], a typical child is catching a cold every month, but is perfectly well in between. Sometimes the symptoms are slight – perhaps a runny nose only, and may go unnoticed, especially in a large busy family. In the lower figure [B], the child with reactive airways gets the same number of colds, but because of their sensitive airways, the symptoms are more pronounced and the cough lingers for longer. The child has not fully recovered before catching the next cold and the parents have the impression the child coughs continuously throughout the winter. They may also forget the brief periods when the child has improved.
All young children cough and many wheeze. This inevitably leads to a visit to the GP and it is not uncommon for these children to receive multiple courses of antibiotics, which enhances the parents’ belief that there is something wrong with their child. Children are often said to have recurrent chest infections, when in reality they are having the usual number of upper respiratory tract infections (viral colds), but with accompanying lower airway symptoms. However with current diagnostic trends, many of these pre-school children are given the label of asthma, which can cause considerable parental anxiety and in a few cases even social stigmatisation. A proportion will also be prescribed inhaled steroids, following the message that inhaled steroids rather than antibiotics are the treatment of choice for these recurrent symptoms.
It is difficult to diagnose asthma in this age group. In the past, these children were diagnosed as having wheezy bronchitis, however use of the term bronchitis led to widespread use of antibiotics, despite the fact that almost all these episodes are caused by viral and not bacterial infections. In an attempt to encourage use of bronchodilators, it was then emphasised that wheezing equals asthma. This inevitably led to over-diagnosis, and with the British Thoracic Society guidelines emphasising the use of inhaled steroids for asthma prevention, many children have been put on steroids unnecessarily. Clearly the pendulum needs to swing back as the truth lies somewhere in the middle. Whilst most asthmatic children cough (and some do so without obvious wheeze), most children who cough do not have asthma. Furthermore, many parents report that their child wheezes, when what they are really describing are the harsh sounds of upper airway secretions in the back of the throat.
So how is asthma diagnosed in this age group? The history is usually the key and there are certain pointers –
• Family history of atopy – asthma, hay fever or eczema in a parent or sibling (ignore the elderly grandparent who has bronchitis).
• Personal history of atopy – genuine atopic eczema rather than the occasional patch of dry skin.
Pattern of wheeze – background daily or night-time symptoms, or exercise-induced symptoms, rather than the commoner pattern of symptoms only when the child has a viral cold.
Examination is usually normal and unhelpful. However the presence of Harrison sulci (indentation or concave shape of the lower ribs) indicates chronic respiratory difficulties and is significant. Plotting height and weight may be useful, as poor growth may indicate a more significant underlying condition such as cystic fibrosis.
Investigations are usually unhelpful. Children under 6 years of age are unable to perform lung function testing, which is unfortunate as spirometry is the best way of confirming the presence of airways obstruction. Although the committed allergist may disagree, skin prick testing in this age group is rarely helpful.
If symptoms are marked or atypical, referral to a paediatrician is warranted, particularly one with a respiratory interest. In some cases, further investigations may be performed to exclude less common diagnoses. Gastro-oesophageal reflux, a condition where stomach acid regurgitates back up the oesophagus (food-pipe) must always be borne in mind, as not uncommonly it manifests as recurrent cough and wheeze that has not responded to standard therapy.
The single best thing most parents could do to help their symptomatic child is to stop smoking. It is our duty to inform the parents of the harm they are inflicting on their children (and themselves). In addition, constructive advice should be given to try and help those who wish to give up the habit.
Bronchoconstricted (narrowed) airways need bronchodilators – but these should only be used on an ‘as required’ basis rather than automatically taken 3-4 times a day. Nowadays they should be administered through a spacer device with a mask. There are several of these available on prescription, smaller volume ones include the AeroChamber and Able Spacer, larger volume ones include the Volumatic and Nebuhaler.
There is no point using this method if a child is distressed and screams every time the mask is put on their face, as drug deposition becomes minimal. In those circumstances, a, nebuliser remains the only option, but fortunately this is not too common an occurrence. By 3 years of age, most children can use the spacer without the attached mask, which increases the efficiency of lung deposition. Bronchodilators given in syrup form are far less effective and probably not worth using, as the dose required orally, in order to have an impact inevitably leads to side effects.
A small minority of pre-school children will require regular prophylaxis. Inhaled steroids are not too effective for those children who have episodic viral wheeze. However in those with background troublesome symptoms who are using a bronchodilator several times a week, a trial of inhaled steroids is warranted. Again, these should be administered through a spacer device, with or without a mask depending on age.
Fortunately the prognosis is generally very good and most will outgrow their symptoms. However, although most wheezy infants do not turn out to have persistent childhood asthma, most asthmatics do start wheezing when young. If we had a reliable predictor of those who will develop asthma with eventual structural changes in the airways, we could then target aggressive early anti-inflammatory therapy. Since currently no such predictor exists, this form of preventive management will have to wait.
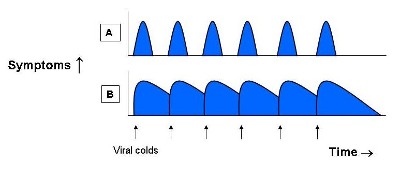
The shaded area represents times when a child is having symptoms, while the arrows represent each viral cold they catch. On average, the pre-school child gets 8-12 colds per year, mostly between September and March. In the top figure [A], a typical child is catching a cold every month, but is perfectly well in between. Sometimes the symptoms are slight – perhaps a runny nose only, and may go unnoticed, especially in a large busy family. In the lower figure [B], the child with reactive airways gets the same number of colds, but because of their sensitive airways, the symptoms are more pronounced and the cough lingers for longer. The child has not fully recovered before catching the next cold and the parents have the impression the child coughs continuously throughout the winter. They may also forget the brief periods when the child has improved.
© Dr. Ian Balfour-Lynn
Powered by LondonWeb
Designed by CrestanaDS