- 0044 (0) 207 351 8754
- [email protected]
- Royal Brompton Hospital - London
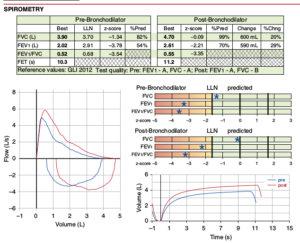
A lung function test gives information on how well the lungs are working. Spirometry measures
the amount of air that can be blown out in the first second (FEV1 – forced expiratory volume in 1st second), and the total amount that can be exhaled (FVC – forced vital capacity). The test can also indicate whether there is obstruction to airflow, as is typically seen in asthmatic children
Reliable measurements can be obtained from children aged 6-7 years and above on.
A simpler test may also be carried out with a peak flow meter which measures the highest flow (PEFR – peak expiratory flow rate) that the child can produce whilst breathing out, and again this may be reduced in an asthmatic child.
No preparation is necessary apart from spitting out any chewing gum!
Lung function tests are usually done during clinic visits and the whole procedure takes about 5 minutes. For spirometry, the child takes a deep breath and then blows as fast and as long as possible into a cardboard tube which is connected to a spirometer (lung function machine). For a peak flow reading, the child takes a deep breath and then blows out as hard as possible for a few seconds. The result is then printed out so is available immediately. The child’s values are compared to those expected for the same age, gender, height and ethnicity. Values above 80% predicted are considered normal.
A spirometer and print out of a result.

A peak flow meter

The test is not uncomfortable but if the child feels breathless at any time they can simply stop blowing. Occasionally children cough a little immediately after the forced blowing.
Sometimes more information is needed than can be obtained from simple spirometry in clinic and these tests are carried out in a lung function laboratory.
An exercise test shows whether a child’s airways tighten (bronchoconstrict) during exercise which leads to a reduced air flow. This is not uncommon in asthmatic children and it is known as exercise-induced bronchospasm.
A bronchodilator responsiveness test tells us whether a child’s airways have the ability to relax (bronchodilate) and thus increase their air flow, when a child inhales a bronchodilator medicine (for example salbutamol). It is almost always combined with an exercise test in the lung function lab, but can be done as a single test in clinic if the child’s lung function is already reduced at rest.
The following should not be taken for 12 hours before the test:
The following should not be taken for 4 hours before the test:
It is worth wearing comfortable clothes and wear trainers for an exercise test.
It is also best not to have a large meal or fizzy drinks just before the test.
You need to allow 1½ to 2 hours for the testing. The lung function laboratory is on the 1st floor of the Brompton Fulham Wing (see map).
Children run on a treadmill (a simple running machine often seen in gyms) and have their heart rate monitored continuously with some sticky pads on the chest. The lung function (FEV1) is measured before the start, then every 2 minutes through the exercise. The test is stopped when the heart rate goes up to a specified level to ensure that the child is exerting themselves to a sufficient degree.
Once the exercise stops, the FEV1 is measured every minute for 5 minutes, then at 10, 15, 20, 30 and 60 minutes afterwards. Measuring stops when the lung function has responded by falling so may not take as long as 30 or 60 minutes.
Once a response is seen, a bronchodilator is given (4 puffs of salbutamol through a spacer device) and the lung function remeasured 15 minutes later to test for bronchodilator responsiveness. If a drop in lung function is not seen after 60 minutes, a bronchodilator is still given at that time.
Bronchodilator responsiveness – if this is being done on its own, then after baseline spirometry, 4-10 puffs of salbutamol are inhaled through a spacer device and lung function measured 15 minutes later.
Children are monitored carefully throughout the test. If they feel symptoms for example a wheeze, tight cough, or uncomfortable chest then the test can be stopped immediately and bronchodilators given. If they feel dizzy or light headed then again they can rest immediately. If they feel generally ‘puffed out’ or have tired legs they may be encouraged to continue if they feel able.
You will be able to go home although occasionally the tests are carried out on the same day as clinic. Results will be sent to Dr Balfour-Lynn who will interpret them for you. A drop of 10% or more in lung function with exercise is considered abnormal. We also measure the lability index (maximum value minus minimum divided by expected) which indicates the variability of measurements, and a value above 22% is abnormal.
Nitric oxide (NO) is a gas that is produced naturally within the lungs. More NO is produced from airways if there is inflammation, for example in asthma or allergy. The test measures the level of NO in the air passages of the lungs. This is a test we can carry out in clinic, your child
Nitric oxide (NO) is a gas that is produced naturally within the lungs. More NO is produced from airways if there is inflammation, for example in asthma or allergy. The test measures the level of NO in the air passages of the lungs. This is a test we can carry out in clinic, your child
© Dr. Ian Balfour-Lynn
Powered by LondonWeb
Designed by CrestanaDS